Immunotherapy: a New Approach of Cancer Treatment
Immunotherapy is a type of oncology treatment that helps the immune system fight cancer. The immune system helps the body fight infections and other diseases. Immunotherapy is a type of biological therapy. Biological therapy (as discussed in earlier publications) is a type of treatment that uses substances made of living organisms to treat cancer.
Immuno-oncology therapy, including checkpoint inhibitors, therapeutic cancer vaccines, cytokines and cell therapies, has revolutionized cancer treatment in the past few years. There is still significant room for improvement in immuno-oncology therapy’s efficacy and safety. Continued research and development efforts are underway around the world, with a focus on characterizing novel immuno-oncology targets and exploring combination therapies.
As discussed in earlier publications, given the substantial number of cancer patient population in China and the US, the global market size for immuno-oncology therapies is projected to continue growth at a substantial rate both domestically in China and abroad.
Several types of immunotherapy are used to treat cancer. These include:
- Immune checkpoint inhibitors, which are drugs that block immune checkpoints. These checkpoints are a normal part of the immune system and keep immune responses from becoming too strong. By blocking them, these drugs allow immune cells to respond more powerfully against cancer.
- T-cell transfer therapy, which is a treatment that boosts the natural ability of T cells to fight cancer. Those that are most active against cancer are selected or modified in the lab to better attack cancer cells.
- Monoclonal antibodies, which are immune system proteins created in the lab, are designed to bind to specific targets on cancer cells. Some monoclonal antibodies mark cancer cells so that they can be better identified and destroyed by the immune system.
- Treatment vaccines, which work against cancer by boosting the immune system’s response to cancer cells. Treatment vaccines are different from the ones that help prevent disease.
- Immune system modulators, enhance the body’s immune response against cancer. Some of these agents affect specific parts of the immune system, whereas others affect the immune system in a more general way.
The most widely prescribed and efficacious single-agent immuno-oncology antibody therapies that have been discovered and successfully developed to date are PD-(L)1 (programmed cell death protein 1 and programmed death-ligand 1) and CTLA-4 (cytotoxic T-lymphocyte-associated protein 4) monoclonal antibodies. In addition to PD-(L)1 and CTLA-4, there are also a number of other immune checkpoints that are being explored in clinical trials.
In this publication, we will discuss PD1 (programmed cell death protein 1) and PDL1s (programmed death-ligand 1) immunotherapy.
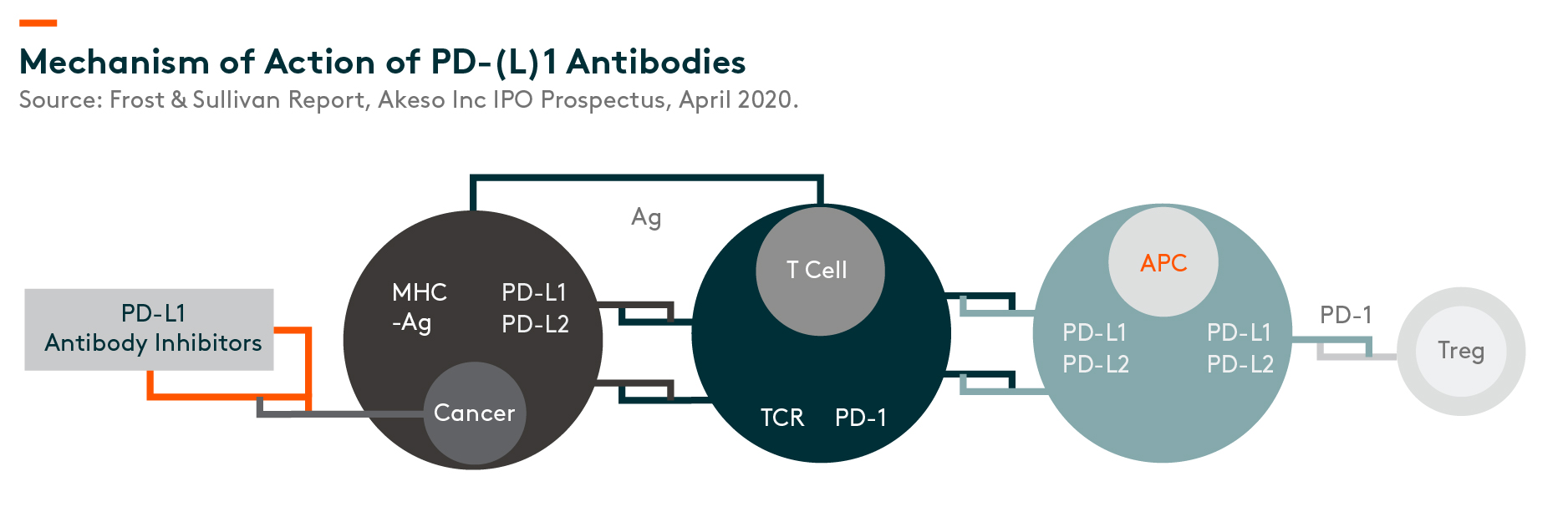
TCR – T-cell receptors, APC – antigen-presenting cells, MHC – major histocompatibility complex, Ag – antigens,
Mechanism of Action MOA
PD-1 is a protein located on the surface of T-cells and is one of the proteins commonly referred to as an “immune checkpoint”. The general function of PD-1 is to prevent the T-cell mediated immune response from attacking normal cells in the body when certain proteins called PD-1 ligand 1 (PD-L1) and PD-1 ligand 2 (PD-L2) on the surface of a normal cell bind to it.
Some cancer cells can express high levels of PD-L1 and PD-L2 to bind to the PD-1 on T-cells and thereby help the cancer cells evade T-cell attacks. PD-(L)1 antibody bind to PD-1 or PD-L1 and blocks PD-1 from binding to PD-L1 and/or PD-L2. This prevents the PD-1 found on T-cells from binding with the PD-L1 and/or PD-L2 found on cancer cells, which allows the T-cells to kill the cancer cells.
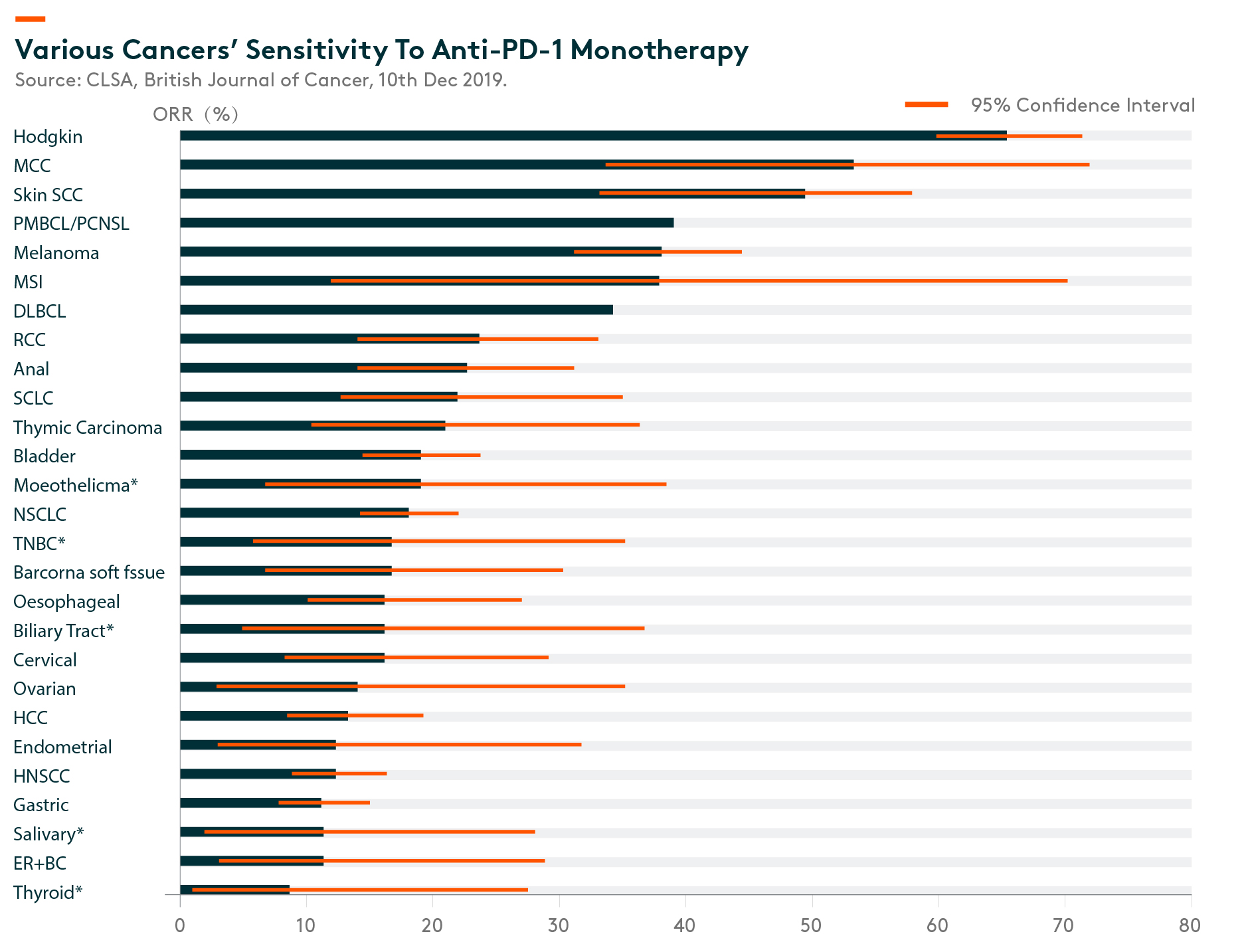
Immunotherapy has demonstrated success in some cancer types, such as Hodgkin’s lymphoma where the response rate is in the 80-90% range, the average response to anti-PD-(L)1 blockade is only around 15-20% in an all-comer population. (CLSA, 10 December 2019) Many solid tumors have low response rates, including some of the high incidences: gastric, head and neck squamous cell carcinoma, hepatocellular carcinoma, ovarian, cervical, biliary tract, esophageal, triple-negative breast cancer, and Non-Small Cell Lung Cancer – Non-Squamous (“NSCLC”), as shown in the below figure.
ORR – Overall Response Rate. Source: CLSA, British Journal of Cancer, 10th Dec 2019. MCC – Merkel cell carcinoma, Skin SCC – Skin squamous cell carcinoma, DLBCL – Diffuse large B-cell lymphoma, RCC – Renal cell carcinoma, SCLC – small cell lung cancer, NSCLC – Nonsmall-cell lung carcinoma, TNBC – Triple-negative breast cancer, HCC – Hepatocellular carcinoma, HNSCC – Head and neck squamous cell carcinoma, ER+ BC – Estrogen receptor Positive Breast Cancer
Globally, there are currently three PD-1 mAbs (monoclonal antibodies) approved by the US-FDA (US Food and Drug Administration) for 17 cancer indications, and three PD-L1 mAbs for six approved cancer indications. In China, there are currently six PD-1 mAbs and one PD-L1 mAb approved by NMPA(National Medical Products Administration). (Source: Akeso Inc IPO prospectus, April 2020).
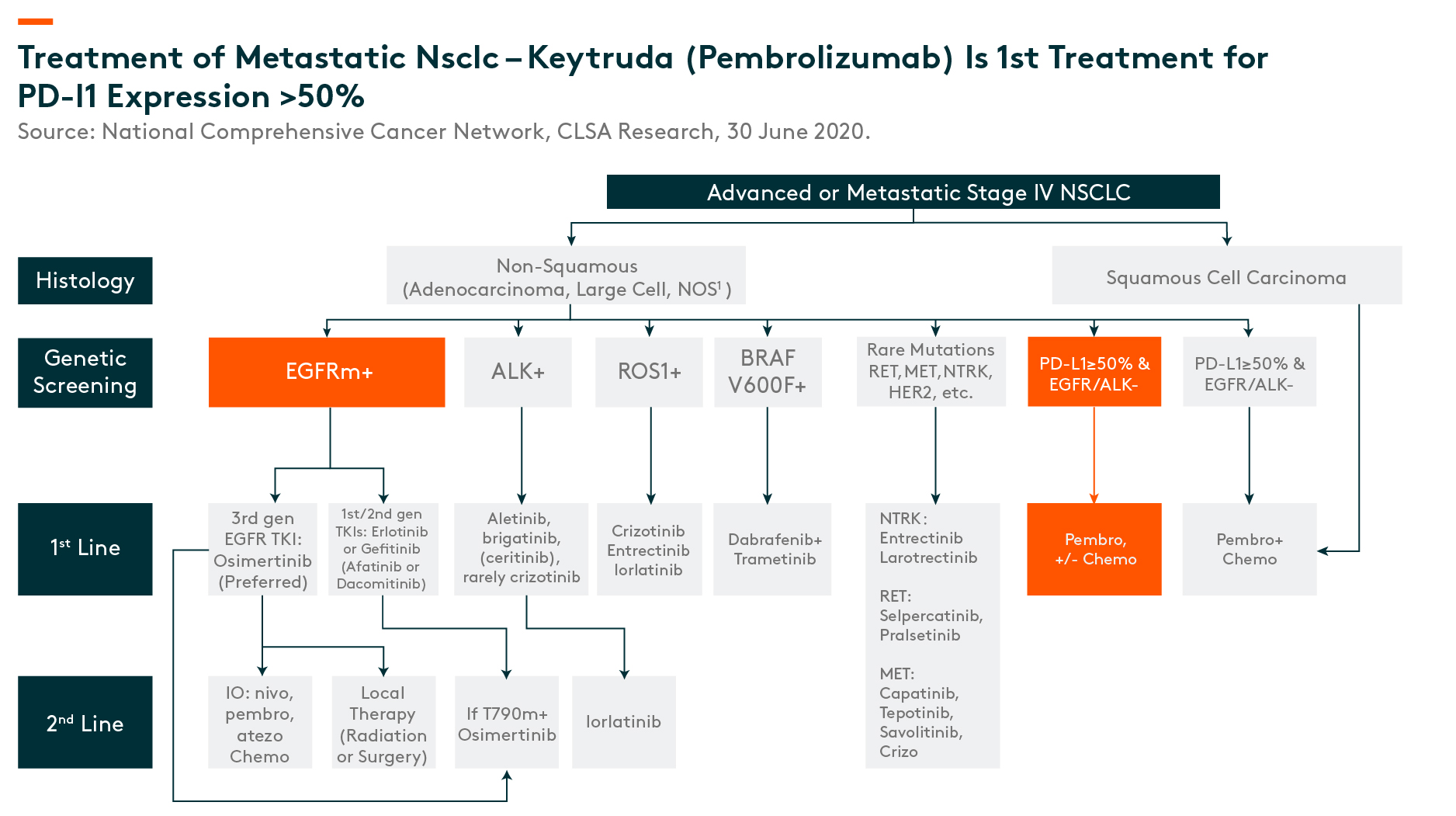
PD1 is becoming the cornerstone of treatment – Example of stage IV NSCLC (Non-Small Cell Lung Cancer – Non-Squamous)
Of all types, lung cancer is the largest oncological indication, with 2.09 million patients per year globally, in 2018. (CLSA, 30 June 2020)_
Globally, PD1 is now considered a standard of care for late stage NSCLC (for patients without any driver gene mutations). As seen in the below chart, if patients have actionable drivers, they are typically given targeted, small-molecule therapies, while among patients without actionable driver mutations (those responsive to targeted therapies), the cornerstone treatment is Keytruda (pembrolizumab1) based programs.
Combination therapy
There is growing recognition in the academic and industry community that immuno-oncology combination therapies that simultaneously employ different mechanisms of action often display improvement in response rate and durability as compared to single-agent immunotherapies. Therefore, we believe that immuno-oncology combination therapies, especially combinations of two or more targeted therapies, are expected to be one of the future trends of oncology therapies.
With clinical evidence of synergy between PD-(L)1 agents and CTLA-4 agents, PD-(L)1 and CTLA-4 combination therapy has in recent years generated tremendous interests from the pharmaceutical industry. Examples of combination therapies include:
- Dual T Checkpoint Inhibitors, eg. PD-1 or PD-L1 together with, CTLA-4, LAG-3 (Lymphocyte-activation gene 3), TIM-3 (T-cell immunoglobulin and mucin domain-3)
- Checkpoint Inhibitors + Costimulatory Receptor Agonists
- Costimulatory Receptor Agonists + Immunomodulators
- Checkpoint Inhibitors + Target Therapy, eg. VEGFR (vascular endothelial growth factor)
- Checkpoint Inhibitors + Immunomodulators/suppressor
- Checkpoint inhibitors + Other Immune System Activators, eg. chemo, IL-2 (Interleukin-2), Vaccines
Beyond PD1s
As immune checkpoint inhibitors become the standard-of-care in many indications, such as lung cancer, more and more patients are progressing through these therapies, creating the need for treatment beyond PD-1/PDL1s.
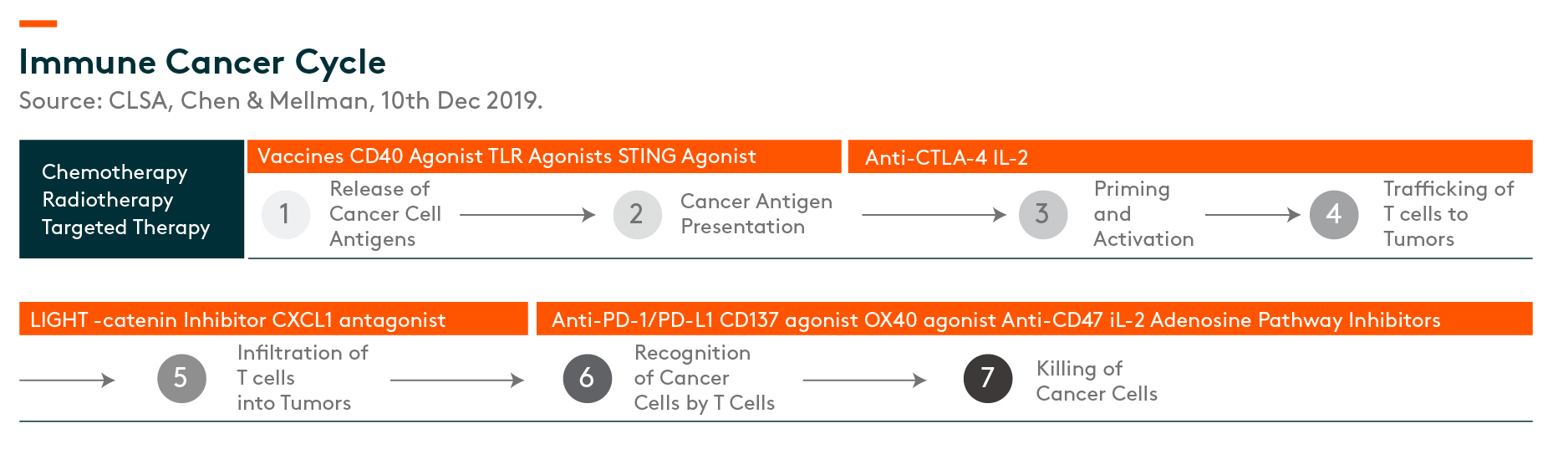
There are several links in the immune cancer cycle that offer potential targets for immune-therapy. PD-1 agents target the last step, the killing of cancer cells, while CTLA-4 class of agents target priming and activation.
Related ETF
Global X China Biotech ETF seeks to provide investment results that closely correspond to the performance of the Solactive China Biotech Index NTR, offering an access high growth potential through companies critical to the development of biotechnology in China.
Other Features
Targeted Exposure: The fund delivers targeted exposure to an emerging theme and industry.
ETF Efficiency: In a single trade, the fund delivers access to dozens of companies with high exposure to the biotech theme in China.
Click here to learn more about our Global X China Biotech ETF.